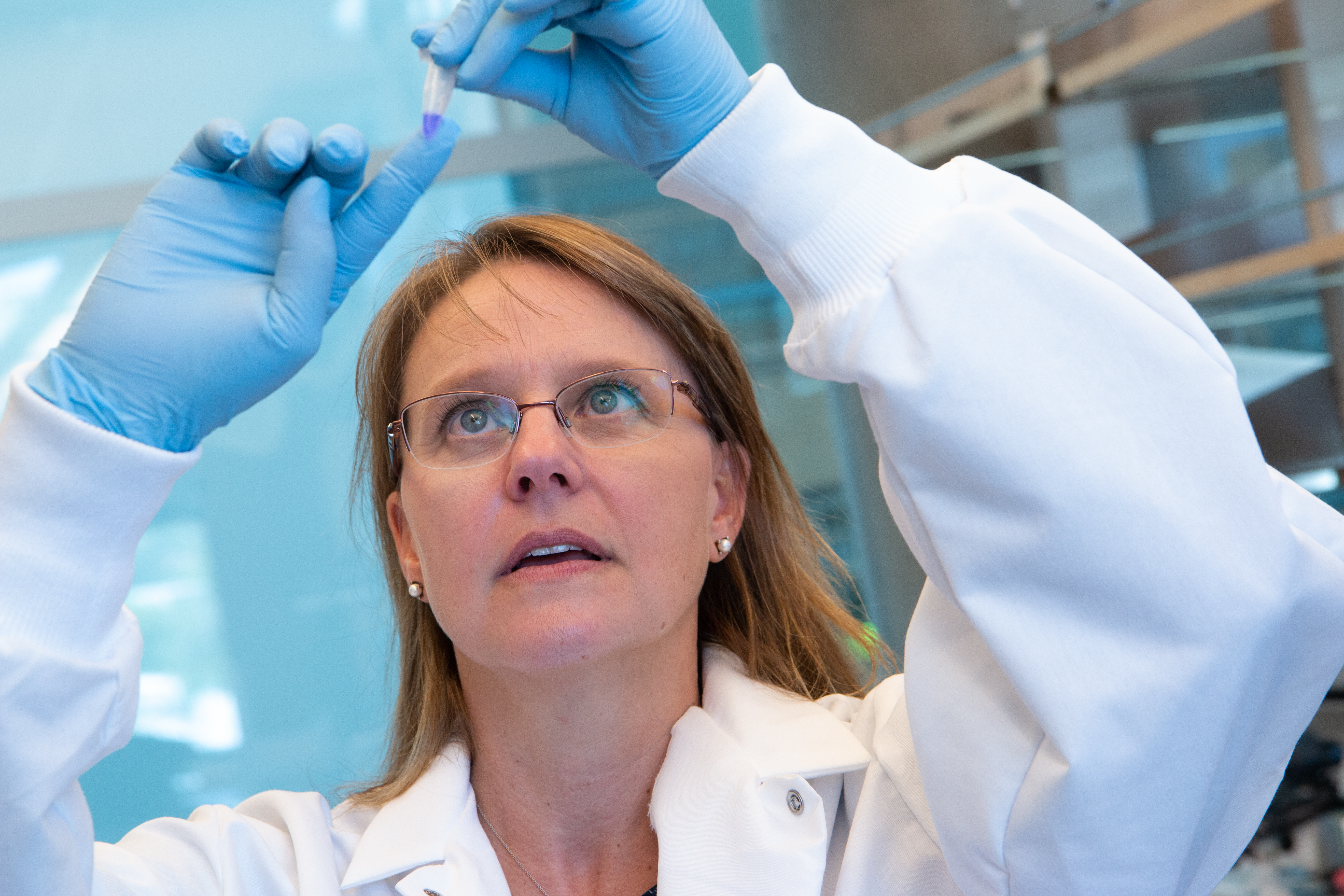
Tara Deans is an Associate Professor here, at the University of Utah Biomedical Engineering Department, whose research focuses on building synthetic gene circuits to reprogram cells. At this year’s European Laboratory Research and Innovation Group’s (ELRIG) Research and Innovation conference (29th–30th March 2023; Cambridgeshire, UK), Tara shared more about what synthetic biology is, and her research engineering platelets to target circulating tumor cells with the aim of preventing metastasis.
See the full interview at BioTechniques here

What is synthetic biology?
Synthetic biology involves putting different genetic parts together, which will change the function of the cell. This is the basis of reprogramming cells. Oftentimes in the field, people talk about genetic parts as being Lego pieces because it’s a little bit more conceptual for people outside of the field. If you move a green Lego piece and a yellow Lego piece in different orientations and even build it on top of other ones, you will get a different function in the cell.
What do genetic circuits consist of?
In electrical engineering, you have a motherboard to which you add resistors and capacitors with the goal of turning on a lightbulb, for example. We do some very similar things in synthetic biology, except our light bulb is gene expression and our parts are DNA or RNA.
We take these individual gene regulatory parts and engineer them into a larger circuit, so these parts interact with each other. Oftentimes they are inducible, so they can be turned off and turned on to give us dynamic expression in cells. To do that, we can either add small molecules or add light. We can also engineer cells to have autonomous reprogramming, where cells execute their new functions based on their cell state or environment. In my talk, I showed that you can use tissue-specific promoters. These are promoters that only turn on when the cell is, in my case, a megakaryocyte, which is the cell that makes platelets. This lets us know when the cell is ready to become a megakaryocyte in the timeline of differentiation.
What techniques do you use to create genetic circuits?
We can use restriction endonucleases to cut and paste DNA pieces together, or have our DNA parts synthesized by companies. There are activators and repressors, which activate and repress gene expression respectively. We use these basic regulatory parts and piece them together to reprogram cells.
Why are you interested in engineering platelets?
We are very interested in making platelets in vitro because platelets have a whole slew of important functions in the body. Most people are more familiar with their clotting function – when you start bleeding, platelets collect and stick together and form a clot so you don’t bleed out – which is very important, but platelets are also extremely important in hemostasis and in regulating the immune system and the cardiac system. They are really, really important cells.
What kind of properties can you engineer megakaryocytes to have?
We are engineering them to target certain cell types, for example, we are interested in circulating tumor cells to try and mitigate metastasis. These are cells that come off of a tumor and go into the bloodstream and then they end up finding a new home, which is the basis of metastasis. Platelets are naturally attracted to circulating tumor cells and they cover them, so the immune system can’t see them, and the immune system has no idea this is going on. They don’t see them at all. Then the circulating tumor cells activate the platelets to release proteins that help the circulating tumor cells to break through from the vessel into a new location in the body.
Because platelets provide this native covering of the circulating tumor cells, we are putting split toxins inside of our engineered platelets. If we put in a full toxin, it would kill the platelet, so we have to split it in half, this results in two separate platelet populations. These proteins are really interesting because they spontaneously come together in the cytoplasm of circulating tumor cells and form a functioning protein, in this case a functioning toxin, which kills the circulating tumor cells. We also have things on the outside of the platelets to further target circulating tumor cells. When the platelets bind to the circulating tumor cells, they are activated and release their half of the toxins into the circulating tumor cell, killing it once the toxin comes together.
What advice do you have for presenting at a conference?
Practice, practice, practice.
Practice in front of different audiences, not just in front of your lab – your lab knows what you are doing, but your audience typically doesn’t. There’s nothing wrong with making your audience feel smart, so it’s okay to tell them something that they probably know because it will keep them engaged and interested like, “Oh my gosh, I know that!” Then, lead into the points that are more unknown to the audience.
Bring your audience with you. Don’t just jump off a cliff and hope they follow.
Try to meet people. I remember when I was young and a trainee, I was terrified to talk to the established people in the field, but everyone is approachable and will talk to you, certainly in synthetic biology. So I encourage people to approach researchers who are established in the field.